By Dr.D.K.Kushwaha BPT/MPT (Neuro) Physiotherapist September 19, 2024
DESCRIPTION-
Total knee joint replacement (TKR) or Total knee arthoplasty (TKA) is a orthopaedic surgical procedure where the articular surfaces of the knee joint (the femoral condyles and tibial plateau) are replaced.
Knee joint replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
If nonsurgical treatments like medications and using walking supports are no longer helpful, you may want to consider total knee replacement surgery. Joint replacement surgery is a safe and effective procedure to relieve pain, correct leg deformity, and help you resume normal activities.
Reasons for a patella replacement include: osteolysis, maltracking of the patella, failure of the implant.
The aim of the patella reconstruction is to restore the extensor mechanism. The level of bone loss will dictate which kind of patella prosthesis is placed.
If the knee is severely damaged by arthritis or injury, it may be hard for you to perform simple activities, such as walking or climbing stairs. You may even begin to feel pain while you are sitting or lying down.
Total knee replacement facts :
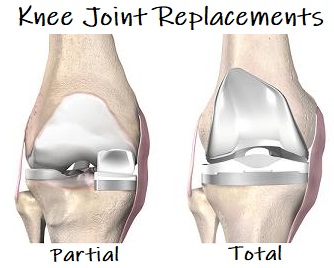
Knee Joint replacement
Patients with severe destruction of the knee joint associated with progressive pain and impaired function maybe candidates for total knee replacement.
Osteoarthritis is the most common reason for knee replacement operation.
Anatomy of Knee Joint :
The knee is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily within the joint.
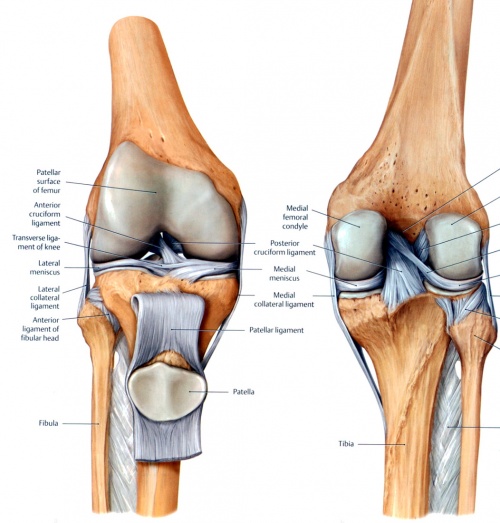
Knee joint image
- Tibiofemoral – medial and lateral condyles of the femur articulate with the tibial condyles. It is the weight-bearing component of the knee joint.
- Patellofemoral – anterior aspect of the distal femur articulates with the patella. It allows the tendon of the quadriceps femoris (knee extensor) to be inserted directly over the knee – increasing the efficiency of the muscle.
- As the patella is both formed and resides within the quadriceps femoris tendon, it provides a fulcrum to increase power of the knee extensor and serves as a stabilising structure that reduces frictional forces placed on femoral condyles.
Ligaments & Joint Capsule
The joint capsule has thick and fibrous layer superficially and thinner layers deeper. This along side the capsule ligaments enhances she stability of the knee. As with all of the structures that from the knee they are under most tension therefore more stable in an extended (closed packed) position in comparison to the laxity present in a flexed position (open packed). Inside this capsule is a specialized membrane known as the synovial membrane which provides nourishment to all the surrounding structures. The synovial membrane produces synovial fluid which lubricates the knee joint. Other structures include the infrapatellar fat pad and bursa which function as cushions to exterior forces on the knee. The synovial fluid which lubricates the knee joint is pushed anteriorly when the knee is in extension, posteriorly when the knee is flexed and in the semi flexed knee the fluid is under the least tension therefor being the most comfortable position if there is a joint effusion
The menisci are located between the femur and tibia. These C-shaped wedges act as “shock absorbers” that cushion the joint.
Large ligaments hold the femur and tibia together and provide stability. The long thigh muscles give the knee strength.
All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony. But disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.
In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement.
Clinical Presentation
Pain is the main complaint of patients’ with degenerated knee joints. At first, pain is felt only after rest periods (this is also called ‘starting pain’) after a couple of minutes the pain slowly fades away. When the knee joint degeneration increases, the pain can also occur during rest periods and it can affect sleep at night. Individuals’ can also complain of knee stiffness and crepitus.
Due to pain and stiffness, function can decline and is manifests as reduced exercise tolerance, difficulty climbing stairs or slopes, reduced gait speed and increased risk of falls.
Diagnostic Procedures in Total Knee Joint Replacement :
The diagnosis of patients requiring total knee joint replacement surgery is mostly symptom-based. Pain, loss of range of motion and functional impairments are mostly considered here.
An orthopaedic surgeon will guide the diagnosis and management process.
Observation
Subjective interview:
-Complaints of pain, deformity, stiffness and/or limp Previous history linked to hip pain (congenital or childhood problems, previous trauma)
Physical examination :
- Standing
- Trendelenberg test
- Gait
- Supine (including leg length)
- Objective observation (posture, deformities, muscle atrophy)
- Range of motion
Indications for Total knee Joint replacement :
-Pain and loss of mobility are the most common preoperative complaints of patients prior to total hip arthroplasty.
-In advanced cases, despite full conservative management, persistent pain, limited mobility and night pain is normally present.
-When there are complications with the internal fixation of a fracture to the femoral neck, in particular, if articular cartilage in the acetabulum is lost or when endoprosthesis has failed in acute fractures, a total hip replacement is a good solution.
Common indications include
- Osteoarthritis
- Post-traumatic arthritis
- Rheumatoid arthritis including juvenile rheumatoid arthritis
- Avascular necrosis
- Hardware failure after internal fixation of hip fractures
- Congenital hip dislocations and dysplasia
Contraindications for Surgery:
Absolute Contraindications
-Active infection in the joint, unless carrying out a revision as either an immediate exchange or an interval procedure.
-Systemic infection or sepsis.
– Neuropathic joint.
-Malignant tumors that do not allow adequate fixation of the components.
Relative Contraindications
- Localized infection, especially bladder, skin, chest, or other local regions.
- Absent or relative insufficiency of the abductor musculature.
- Progressive neurologic deficit.
- Any process rapidly destroying bone.
- Patients requiring extensive dental or urologic procedures, such as transurethral resection of the prostate, should have this] [performed before total joint replacement.
Possible Complications of Surgery
-Stiffness is the most common complaint following primary total knee replacement, affecting approximately 6 to 7% of patients undergoing surgery.
- Loosening or fracture of the prosthesis components
- Joint instability and dislocation
- Infection
- Component misalignment and breakdown
- Nerve damage
- Bone fracture (intra or post operatively)
- Swelling and joint pain
- Complications as above may require joint revision surgery to be performed.
Physiotherapy Management
Pre-operative in Total knee joint replacement :
The physiotherapist can choose to teach the patient the exercises before surgery in order that the patient might understand the procedures and, after surgery, be immediately ready to practice a correct version of the appropriate exercises. It is also important that the functional status of the patient before surgery is optimised to assist recovery. The focus of a pre-operative training program should be on postural control, functional lower limb exercises and strengthening exercises for both of lower extremities.
Post-operative
-The most important role of physiotherapists in the management of patients following TKA is facilitating mobilisation within 48 hours of surgery, sometimes as early as the same day as the operation (Day 0). The use of a continuous passive motion (CPM) may be utilised in this period.
cryotherapy improves knee range of motion and pain in the short-term
Common Bed and Chair Exercises:
- Ankle plantarflexion/dorsiflexion
- Isometric knee extension in outer range
- Inner Range Quadriceps strengthening using a pillow or rolled towel -behind the knee
- Knee and hip flexion/extension
- Isometric buttock contraction
- Hip abduction/adduction
- Straight leg raises
REHABILITATION PROCOL
Phase I – Immediate Post Surgical Phase (Day 0-3):
The goal of physical therapy intervention during the early post-operative phase is to decrease swelling, increase range of motion, enhance muscle control and strength in the involved lower extremity and maximize patients’ mobility with a goal of functional independence. Physical therapy interventions are also directed towards identifying other sensomotor or systemic conditions that may influence a patients’ rehabilitation potential.
Therapeutic exercise and functional mobility:
• Active/active assisted/passive (A/AA/PROM) exercises (seated and supine).
• Patella femoral and tibial femoral joint mobilization and soft tissue mobilization as
indicated.
• Soft tissue massage.
• Isometric quadriceps, hamstring, and gluteal isometric exercises.
• Straight leg raises (SLR)
• Lower extremity range of motion (ROM) and strengthening as indicated based on evaluation findings.
• Closed chain exercises (if patient demonstrates good pain control, muscle strength and balance). Close-chained exercises should be performed with bilateral upper extremity support while maintaining appropriate WB precautions.
• Gait training on flat surfaces and on stairs.
• Transfer training.
Active/active assisted/passive (A/AA/PROM) exercises (seated and supine).
• Patella femoral and tibial femoral joint mobilization and soft tissue mobilization as
indicated.
• Soft tissue massage.
• Isometric quadriceps, hamstring, and gluteal isometric exercises.
• Straight leg raises (SLR)
• Lower extremity range of motion (ROM) and strengthening as indicated based on evaluation findings.
• Closed chain exercises (if patient demonstrates good pain control, muscle strength and balance). Close-chained exercises should be performed with bilateral upper extremity support while maintaining appropriate WB precautions.
• Gait training on flat surfaces and on stairs.
• Transfer training.
• Patients are encouraged to use cryotherapy for 20 minutes before and after their independent exercise program.
Phase II –Motion phase [Weeks 1-4]:
AA/A/PROM, stretching for flexion (>90 degrees) and extension
• Stationary Bicycle for ROM, begin with partial revolutions then progress as tolerated to full revolutions (no resistance).
• Patella femoral and tibial femoral joint mobilization as indicated.
• Continue isometric quadriceps, hamstring, and gluteal isometric exercises
• Supine heel slides and seated Long Arc Quad (LAQ)
• SLR in 4 planes (flexion, abduction, adduction, extension)
Weeks 4-6
• Continue exercises listed in Phase II with progression including resistance and repetitions. It is recommended to assess hip/knee and trunk stability at this time and provide patients with open/closed chain activities that are appropriate for each patient’s individual needs.
• Continue patella femoral and tibial femoral joint mobilization as indicated.
• Initiate endurance program, walking and/or pool.
• Initiate and progress age-appropriate balance and proprioception exercises.
• Discontinue NMES of quads when appropriate quad activity is present.
• Continue above exercises
• Continue patella femoral and tibial femoral joint mobilization as indicated.
• Continue NMES of quads if poor muscular performance of quad is present. May progress NMES use from isometric quad activity to isotonic and functional activity
• Front and lateral step up and step down.
• 1/4 front lunge.
• Use sit to stand and chair exercises to increase knee flexion during functional tasks.
• Continue stationary bicycle for ROM
• Begin pool program if incision is completely healed
Phase III – Intermediate phase (week 7-12):
Phase IV – Advanced strengthening and higher level function stage (week 12-16):
Enhance strength, endurance and proprioception as needed for activities of daily living and recreational activities.
Continue previous exercises with progression of resistance and repetitions.
• Increased duration of endurance activities.
• Initiate return to specific recreational activity: golf, doubles tennis, progressive walking or biking program.